Nursing Facility Transition
to Assisted Living or Home
January 1, 2023 launched this important program for Medi-Cal Recipients throughout California.
- Great news for Medi-Cal recipients and families who wished there was an alternative to Skilled Nursing Long-Term stays.
- Exceptional news for Skilled Nursing Facilities struggling with challenging long-term discharges who are appropriate for lower levels of care.
- Welcome news for Assisted Living Providers who are interested in a fresh pipeline of carefully-matched prospects without the restrictions of ALW and without placement fees.
The Need for Master•Care
By 2025, over 15 million Americans will be "Super Seniors" (over the age of 80.) By 2045, that number will have doubled, representing over 8% of the U.S. Population.
As Baby Boomers age, it will become critical to better manage their healthcare consumption... particularly that of "High (medical) Utilizers."
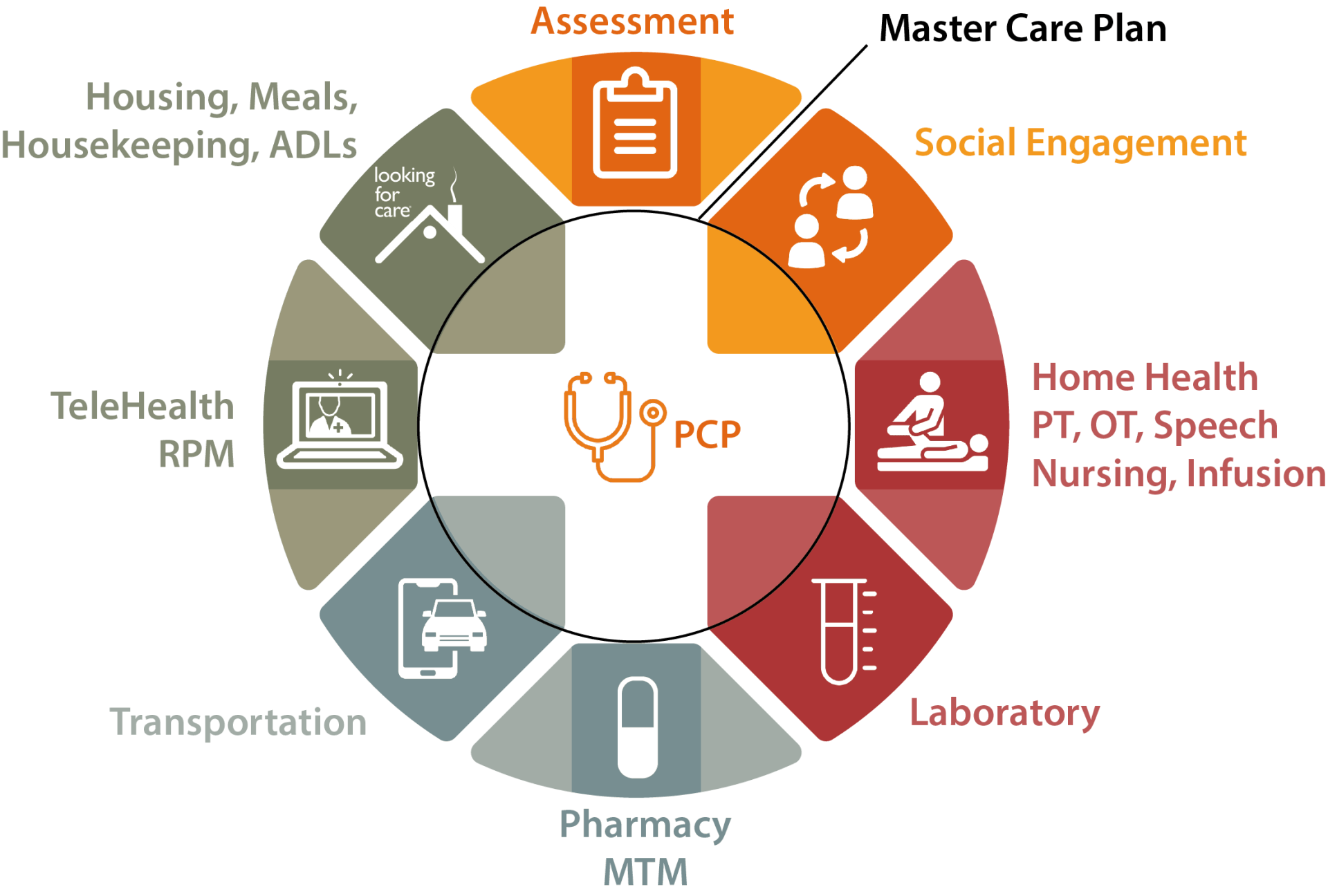
Often health and well-being are significantly impacted by lack of access to "Social Determinants of Health." These non-medical services can be as simple as medication management, or installing grab bars into a shower, but can have a huge impact to improve quality of life and reduce the financial burden of frequent E.R. visits, hospital admissions and custodial skilled nursing care.
If the home environment is unsafe or unsupported, ultimately the health and well-being of a Medicare or Medi-Caid recipient will be adversely affected.
In January 2022, CalAIM launched in California and ushered in a new age of blending clinical oversight with non-medical services. Managed Care Plans and Medi-Caid have recognized the need to cover Social Determinants of Health. These non-medical services (called "Community Supports" in CalAIM) are recommended on a case-by-case basis through a program of "Enhanced Care Management."
Master•Care is an Enhanced Care Management and Community Support provider in multiple California counties and is contracted with multiple Managed Care Plans.
As a bridge between the healthcare world, the private-pay world and the Managed Care world, Master•Care helps bring together needed services — on a case-by-case basis — to improve outcomes and reduce financial burden.
Transitions out of SNF • Reduce Acute Admissions • Reduce E.R. Visits
Maintain Medi-Cal Members Highest Level of Independence
For Managed Care Plans
Value-Based Compensation for Enhanced Care Management and
Community Supports
Partner with the premiere ECM and CS provider focused on statewide and nationwide coverage and Value-Based Compensation.
- Comprehensive wrap-around Care Management system, successful multi-touch Outreach programs and a thorough understanding of local Community Supports.
Reduce High Utilization
Care Navigators help to safely transition challenging members with complex care needs. Care Navigation Teams co-create Immediate, Short-Term and Long-Term Goals with the member and monitor these needs and more:
- Medical (including Pharmaceutical and Dental)
- Social
- Behavioral
- Environmental
- Financial